When you're pregnant a big part of your birth plan is choosing where you'd like to give birth. There are a few options available, including at a hospital, at home, or at a midwife-led birthing centre.
Midwife-led units are staffed entirely by midwives, unlike traditional obstetric labour wards where doctors and anaesthetists are present.
Almost half of pregnant women should give birth away from traditional labour wards, according to guidance from the National Institute for Health and Care Excellence on intrapartum care for healthy women and babies - which recommends women with low-risk pregnancies have a home birth or use a midwife-led unit rather than going to a labour ward.
What is a midwife-led labour unit?
There are two kinds of midwife-led birthing centres: stand-alone birth centres and wards attached to hospitals. In both cases, all care is carried out by midwives who are experts in childbirth with all the skills to help you deliver your baby in a straightforward pregnancy.
You may also hear them called Community maternity units (CMUs), birthing units or midwifery units.
There are usually no anaesthetics available on a unit staffed by midwives, although some may offer pethidine. Pain relief is provided with gas and air and, in many cases, birth pools. The aim is to help women to have a natural labour with no medical intervention, which can lead to less trauma for mother and baby and a shorter recovery period. They aim to offer a more homely environment to give birth, to help you feel calm and more at ease.
There are usually no anaesthetics available on a midwife-led unit, although some may offer pethidine
Midwife-led units could minimise stress
Where you choose to have your baby will influence how relaxed you are in labour. And feeling calm and safe is essential to a labour progressing well. So a labour room that feels like a home from home could help you have a positive birth experience.
When labour starts, your body produces oxytocin, which shapes the frequency, length and strength of your contractions. If you start to feel stressed or anxious, the oxytocin level will drop and your body will produce hormones such as adrenaline, which reduce blood flow to the uterus and slow down the first stage.
Labouring in a tranquil environment also allows you to focus on your body and the baby.
‘The ethos is to normalise the location so it is less like the hospital environment you go to when you are ill,’ says Jane Munro of the Royal College of Midwives.
Women who have used midwife-led units describe them as being like a private hospital
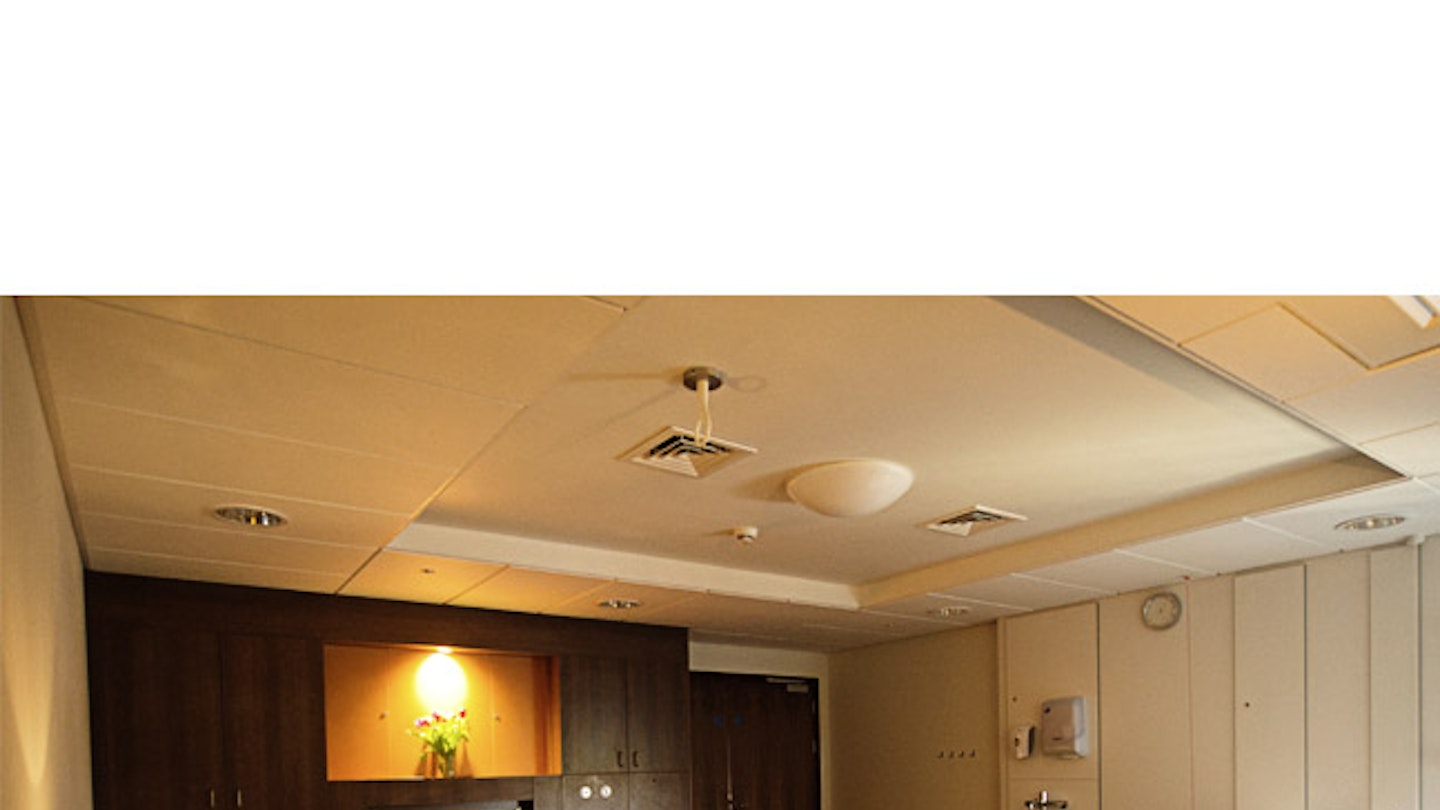
You have a room to yourself, usually with a double bed so your partner can stay, along with an ensuite and sometimes a kitchen area. The walls may be painted in pastel colours, gentle mood lighting and surround-sound speakers helping to complete the atmosphere. Women and birth partners who have used midwife-led units describe them as being like a private hospital, with high levels of maternity support and the chance to stay in the room for a day or two after the delivery.
‘The focus is on comfort, with sofas and beanbags, so you can try different positions during labour,’ adds Jane. ‘They are more hotel-like.’
Offering improved care
There are about 160 midwife-led units in England, of which 6o are freestanding and the other 100 are alongside units at hospitals.
Northampton General opened a midwife-led ward in December 2013 which, in its first year, handled 530 births. It was the first alongside midwife-led unit in the county.
‘The mums love it,’ says matron and intrapartum care lead midwife Paula Briody. ‘When you first book into the hospital with a midwife she will talk through your choices of where you can labour.
"If your pregnancy is low-risk, using the midwife-led ward is offered as an option. If you’re still low-risk by 34 weeks we send the referral. You have to be 37 weeks to deliver here.’
Birthing rooms are geared up for multiple types of birth including water births.
Are birthing centres safe?
According to the NHS you may need to be transferred to a hospital if there are any complications. The Birthplace study found that approximately 4 in 10 women having their first baby in a midwifery unit or birth centre were transferred to hospital, compared with approximately 1 in 10 women having their second or subsequent baby.
In a unit that's completely separate from a hospital, you won't be able to have certain kinds of pain relief, such as an epidural. So, if you are considered as high-risk, or you've had complications in a previous pregnancy, your doctor or midwife may feel it's safer for you to give birth in hospital. Some birth centres won't accept you if you're over a certain age, either.
But having your baby in a birth centre is no more or less risky than in hospital. If you're a first-time mum, having your baby at a birth centre is slightly safer than giving birth at home. Rates for serious problems during labour and birth in the UK are very low, so wherever you have your baby, it's highly likely to be a safe experience.
Birthing centre vs hospital
Many women who use Northampton’s midwife-led units are first-time mums-to-be. They are drawn to the home-from-home atmosphere, but value the safety net of the medical staff close by. This means they can quickly transfer to the medical labour ward if they want an epidural or if there is a complication.
‘If you are having a baby at home and there are complications, there’s a delay if you have to travel to hospital,’ says Paula. ‘A true obstetric emergency is rare. There may be a transfer to the labour ward if there’s meconium (baby’s first faeces) in the amniotic fluid when the waters break or the progress of the labour is slow.’
It’s your choice
‘The deciding factor for most women about choosing where they give birth is where they will feel most comfortable and safe,’ says Jane Munro. ‘For some women this is home, for some it’s a hospital and for some it’s a midwife-led unit.’
Whether you choose a hospital birth or not, your midwife will be able to talk through the options with you and be honest with you about what is a realistic birth choice.
How to find a UK birthing centre near me
To find out about midwife-led units near you, or to choose which birth centre you'd like to use, ask your midwife or visit birthchoiceuk.com for information about local maternity units.