Part 1: Introducing me, my wife, and our conception journey
Hello!
Welcome to my first weekly blog on impending fatherhood.
I’m Jim, my wife’s name is Daisy, she’s 11 weeks pregnant and we’re rapidly coming up to our first major scan where we get to check if everything has gone ok in the first trimester.
All being well, this will be our first child.
I guess the aims of this blog over the coming months will be threefold:
-
To diarise what happens in my journey toward becoming a dad for the first time
-
To try and convey what I learn through the experience
-
To attempt to give advice to and empathise with those who may need it
I’ll cover all sorts of subjects: how Daisy and I are coping mentally and the worries we will face together. The things I learn about pregnancy and the birthing process. How it may affect our careers and lives.
And then – fingers crossed – I’ll write about whatever happens in the months after the birth.
It will be a proper, ‘in real life’ read from a man's perspective. Maybe not a Nobel literature prize-winning read, but honest to the core and at times, I hope, humorous.
Whatever happens, good or bad, funny or absolutely not very funny at all, you’ll get to read it here.
Why I'm a geriatric dad
Why call this the ‘Geriatric Dad Blog'?
Simple really: I turn 50 in September.
Fifty!
While I still feel like I’m 21, medically my age puts me a tad on the old side to be a father. Most of my friends’ kids have grown up already. My best mate’s daughter is currently on a gap year touring South America and my goddaughter will turn 18 in December.
And – although it was a different era – when my dad was my age, I was 25!
In traditional terms, I suppose by now I should be a granddad as opposed a new dad.
So why have we decided to have a baby now?
The simplest answer is, because it’s the right time. Both myself and Daisy, who’s about to turn 37 and has a successful career as an airline pilot, realise we can’t wait any longer. It’s now or never.
We’re both acutely aware that our age means there is increased risk associated with pretty much everything to do with pregnancy.
Increased risk of the baby being born with various conditions, increased risk of miscarriage (as much as a 25% chance in the first three months of pregnancy, which was a scary figure when I found out about it) and an increased risk to Daisy’s health.
Our 12-week scan is in two weeks (13 April) and we’ll no doubt find out more then about how things are then.
Conception: a wannabe dad's perspective
I’ll return to the subject of scans in next week’s blog.
Today though, I thought I’d talk about my conception experience.
I’ll talk frankly, so if you’re of a sensitive disposition, think twice before carrying on reading!
We were relatively lucky in that it took us slightly less than a year to conceive. In reality, that’s not unusual; though I have to admit that as much as I fancy my wife, the whole conception process for me turned into a bit of a struggle a few months in.
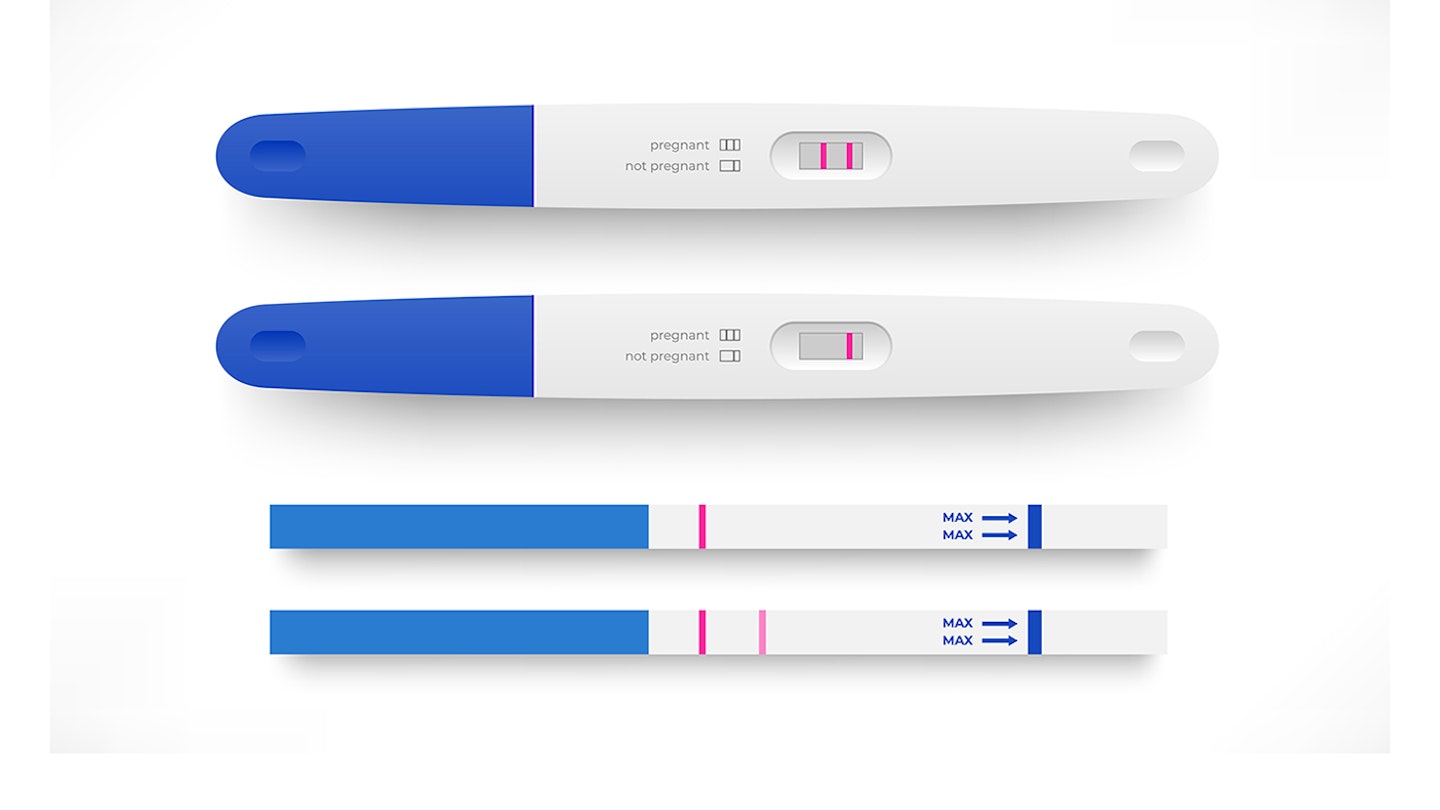
The starting point of it all was for Daisy to test her LH levels (LH = luteinizing hormone) regularly though each menstrual cycle, looking out for rises that could indicate imminent ovulation.
Every day, starting a week or so after her last period, she’d wee on a test stick. She’d do this at home, at work, everywhere. Then, when the hormone levels were at their highest, we’d have an indication as to when the optimal time to conceive might be.
Daisy would even test at work, which isn’t easy while flying a plane at 38,000 feet. When she needed a wee, she’d hand over control to her co-pilot and pop to one of those cramped toilets before whipping out a testing strip to urinate on.
On one occasion, while halfway back from Tenerife, the test indicated she was about to ovulate. She tells me she was tempted to radio air traffic control from the cockpit and ask for a priority landing at Stansted, just so she could get back home asap for a bit of well-timed love-making!
Month after month, it was the same process.
Test, test, test.
Then, typically: “Oooh! Babe! My levels are increasing!!! We MUST have sex NOW!”
One time, I took a frantic phone call when I was in a meeting with some web developers about the merits of CSS code in app builds:
“BABE!
GET HOME NOW!
I.
AM.
OVULATING!”
I’m not sure if my colleagues heard, but they did give me some quite quizzical looks.
It was sometimes hard to get hard
While all this was fun to begin with (the stereotype = it’s every man’s dream to have a beautiful wife constantly demanding sex, and lots of it) it soon became ‘not so much fun’.
As time meandered on, and I am being honest here, sex just became a process – a mechanical event where romance was removed. It became a necessity as opposed spontaneous, enjoyable and romantic.
I realise us men aren’t all the same, but I quickly found I just couldn’t perform as Daisy expected me to – ie, multiple times a day, day after day after day.
In her opinion, this was needed to give us the best chance of conceiving. The more of my sperm was inside her, the more chance it had of meeting an egg.
I disagreed. And besides, I just felt I couldn’t do it.
I might have been able to 30 years ago, but time takes its toll, and these days I’m more of a classic car than a boy racer. Which means I need more maintenance than I used to, more time to get my engine warm, and I need to take care of myself because there’s a bigger risk of breakdown!
Soon, rather than look forward to sex, I started to dread the “I AM OVULATING!” phone call or WhatsApp message.
A woman does not necessarily need to be sexually aroused to physically have sex and conceive (though it helps if you are: some scientific studies apparently reckon it improves your chances of conceiving if you both have strong orgasms!)
But a man? If your body parts aren't working as they should and you can’t get or maintain an erection, baby-making can be a touch problematic.
And that leads to pressure.
Feelings of heavy anxiety started to weigh up inside me as each ovulation approached. Would I be able to perform? Was I producing a big enough volume of sperm? Had the long-term medication I’d been taking for my hypertension affected my fertility?
If I couldn’t do it, what would that mean for our marriage?
The potential ramifications of it all built up and up in my mind, so much so that I soon struggled to get and maintain erections a couple of days into each sex-cycle.
For the first time in my life, I had erectile dysfunction. I felt ashamed, a failure.
It became such a big problem that I ended up going to see my GP.
He asked some awkward questions, checked me out, ran some bloods, got the results (my testosterone levels were apparently fine) then prescribed some special ‘blue’ pills.
He told me it was likely ‘just a mental block’ that was creating difficulty, not anything physical. My bloods were all great. My dangly bits, he said, looked fine (even if he didn't get to see them 'operationally', if you get my drift!)
The pills – basically, Viagra – he said, should work.
Talking problems through with your partner
Rather than bottle all this in, I would definitely advise that, if you’re going through a similar process and problems, you speak with your partner and be searingly honest with each other.
So, Daisy and I talked.
A lot.
And once I’d explained my anxieties and how I was feeling, she became incredibly supportive.
In the end, we agreed a good compromise would be to try to have sex a maximum of once a day over the key probable ovulation days; then outside of that short window maybe once every two to three days.
This, combined with the special pills, seemed to work and one cold morning in January, after getting up for her first wee of the day at 5am, Daisy did a pregnancy test.
After all the failed attempts – all the usual “It’s negative” announcements accompanied with tears, followed by the “Nevermind darling, maybe next time,” response from me – she thought she could see a second line on a test strip (one of those cheap tests bought off Amazon).
She showed me.
“Nah, nothing there,” I said, before switching the torch on my phone on to have a closer look.
“Ummm. Actually, maybe there is something. But it might just be an indent in the card, rather than a positive result.”
I took out some other test strips, unused ones, and had a look at them, holding them side-to-side with the used test.
There was definitely a line. Very faint, but a line all the same.
“YOU DO A TEST!” Daisy said suddenly. “You do one! If a faint line appears on yours, we’ll know it’s just an indent on the strip that’s there from the manufacturer.”
I must be one of the only men in the world to have ever done a pregnancy test. But I did it, and sure enough, nothing appeared. No faint line, no indent, nothing.
Was Daisy finally pregnant? It seemed she might be…
-
The pregnancy is confirmed, despite failing ClearBlue testing kits
-
Jim upsets Daisy with his reaction to a firm positive result!
-
Going for a viability scan at 6 weeks
-
Dealing with anxiety in the first trimester