There’s plenty of things we may get during pregnancy, from the common cold to constipation, or even piles, but pregnancy and chickenpox is particularly nasty.
If you’re not immune to chickenpox, then catching it while you’re pregnant can cause complications for you and your baby. However, there are things that can be done if you do happen to catch it.
Here’s our full guide on how to tackle chickenpox during pregnancy, with some expert advice from Lesley Gilchrist, registered midwife and co-founder of My Expert Midwife.
What is chickenpox?
Chickenpox is a viral infection that causes a rash of itchy, red spots to break out all over your body. It’s caused by a virus called ‘varicella-zoster’ which spreads easily and quickly from person to person and usually clears up on its own within one to two weeks.
Children under the age of 10 are most likely to get chickenpox, whereas adults are more immune to it as they’re likely to have had it before.
What are the symptoms of chickenpox?
While an itchy, spotty rash is the main symptom to look out for with chickenpox, the NHS says the virus usually occurs in three stages, so here’s what to look out for:
Small spots will start to appear - this can be anywhere on the body (including your mouth and genitals).
The spots then become blisters - this is when the spots can become itchy, they fill with a fluid and may even burst.
They turn into scabs - the sport will turn into a scab and may leak fluid or become flaky.
Other symptoms to look out for include:
• A high temperature
• Loss of appetite
• Feeling achy and generally unwell
Can chickenpox during pregnancy cause problems for me and my baby?

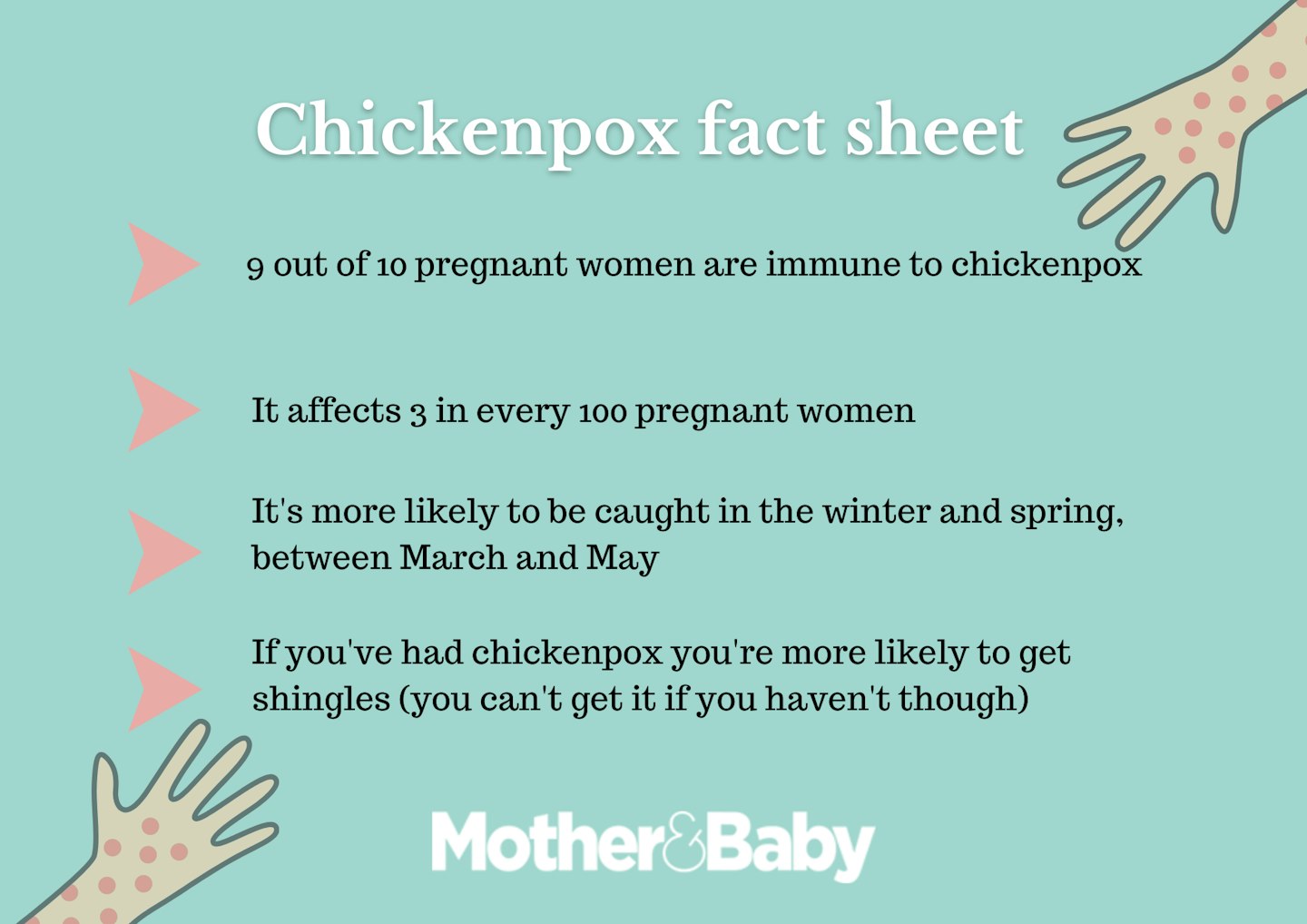
“Nine in ten pregnant women in the UK will be immune to chickenpox and, therefore, they and their unborn baby should be protected during pregnancy," says Lesley.
“If a woman who is not immune to chickenpox becomes infected with it in pregnancy, there could be an increased risk of complications for her (for example, pneumonia, hepatitis or, even encephalitis) and her baby who, depending on the stage of pregnancy when infection occurs, could possibly develop congenital varicella syndrome, or be at increased risk of developing pregnancy shingles or be born with an infection. Although these are rare.”
How is chickenpox treated during pregnancy?
“If you are infected with chickenpox during pregnancy you should always seek medical advice; the treatment will depend on your symptoms and your gestation," explains Lesley. "You may be advised to simply relieve your symptoms with paracetamol, increase fluid intake, and use cooling creams or gels which you can get over the counter.
“However, you may be advised to take antihistamines, but only do so if prescribed or recommended by a GP, pharmacist or nurse practitioner who knows you are pregnant. Alternatively, you may be offered an antiviral medication, called Acyclovir, which lessens the symptoms of the virus but does not cure it.
“In the rare case you develop serious complications, such as difficulty breathing, chest pain, severe headache, extreme lethargy, nausea, vomiting, or an extreme rash or a rash that is bleeding, then you should attend hospital for specialist care.”
How is chickenpox treated after pregnancy?
“After birth, your baby may need treatment with chickenpox antibodies (varicella zoster immune globulin) if you developed a chickenpox rash either within the seven days before or within the seven days after your baby was born. You also need it if your baby has been exposed to chickenpox or shingles within seven days following their birth. If your baby does develop chickenpox, your GP or baby doctor may decide to treat them with an antiviral medication, Acyclovir, to lessen their symptoms.
In very rare cases Lesley says your baby may develop a very serious condition called neonatal varicella. "Early identification and treatment is crucial to ensure your baby’s wellbeing. If your baby was born before 37 weeks of pregnancy, they could be at increased risk of complications from chickenpox and so must be reviewed urgently.”
If you aren’t immune from chickenpox during pregnancy how can you protect yourself?
If you can't confirm whether you are immune to chickenpox - that you have had chickenpox previously or had the varicella vaccination - don't worry, your midwife or GP can check your status with a blood test.
“If you are thinking about pregnancy but not yet pregnant and are not immune to chickenpox, the varicella vaccine is advised," says Lesley. "This is comprised of two doses, with the second dose ideally being given at least three months before getting pregnant. As there is not enough evidence yet on the safety of receiving the vaccine during pregnancy, pregnant women in the UK are currently being advised to consider having it post-delivery, and to stay away from anyone with chickenpox or shingles to reduce the risk of infection.
"If you are pregnant, not sure if you are immune and you come into contact with chickenpox, tell your healthcare provider immediately. You can receive medication that contains chickenpox antibodies which may prevent the infection or reduce your symptoms.”
